Fractures in Children are a common occurrence due to their active lifestyles and developing bones. While fractures can be distressing for both children and parents, the good news is that most fractures can be effectively treated with proper medical care and physiotherapy. This article explores some of the common fractures in children and how physiotherapy plays a crucial role in their recovery.
What are fractures?
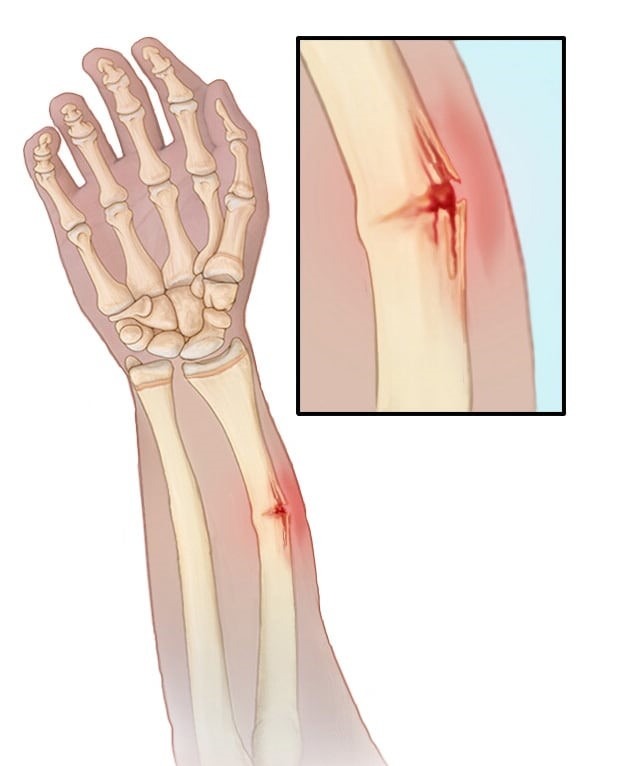
A fracture is a break, usually in a bone. If the broken bone punctures the skin, it is called an open or compound fracture. Fractures commonly happen because of car accidents, falls, or sports injuries. In children, most fractures occur in the wrist, the forearm, and above the elbow.
Causes of Fractures
Fractures in children can occur due to various causes, including:
- Falls: One of the most common causes, children can fracture bones when they fall from playground equipment, bicycles, or while playing.
- Sports Injuries: Participation in sports and recreational activities can lead to fractures, especially in contact sports like football or activities that involve high impact, such as skateboarding.
- Motor Vehicle Accidents: Car accidents and pedestrian accidents can result in fractures in children, especially if they are not properly restrained in car seats or seat belts.
- Playground Accidents: Equipment on playgrounds, like swings, slides, or jungle gyms, can be a source of fractures if children fall or get caught while playing.
- Child Abuse: Unfortunately, child abuse can lead to fractures in children, particularly when there is physical abuse involved.
- Overuse or Stress Fractures: In some cases, children who participate in repetitive, high-intensity activities like gymnastics or long-distance running may develop stress fractures over time.
- Medical Conditions: Certain medical conditions, such as brittle bone disease (osteogenesis imperfecta) or bone tumors, can make children more susceptible to fractures.
- Accidental Trauma: Accidents at home or while playing with objects, like a heavy object falling on a limb, can cause fractures.
- Genetic Factors: Family history and genetics can play a role in bone density and fracture risk.
- Osteoporosis: In rare cases, conditions that affect bone density, like juvenile osteoporosis, can lead to fractures in children.
Symptoms of Fractures
Symptoms of fractures in children can include:
- Pain: The child may experience significant pain at the site of the injury.
- Swelling: Swelling, bruising, or redness may be visible around the injured area.
- Deformity: There could be an obvious deformity or misalignment of the injured limb.
- Limited mobility: The child may have difficulty moving or using the injured limb.
- Tenderness: The area around the fracture may be tender to touch.
- Guarding: The child might protect or hold the injured limb in an unusual way.
- Inability to bear weight: If it’s a lower limb fracture, the child may be unable to put weight on it.
- Crying or distress: Younger children may cry or be irritable due to the pain.
- Numbness or tingling: In some cases, there may be numbness or tingling in the injured area, which could indicate nerve involvement.
What are the types of fractures in children?
Greenstick Fracture
This type of fracture occurs when the bone bends and partially breaks, resembling a green stick that has been bent. A greenstick fracture is a partial bone fracture that occurs in young, still-developing bones. Unlike complete fractures where the bone breaks entirely, in a greenstick fracture, the bone bends and partially breaks, much like a green twig that doesn’t snap all the way. This happens because the bones of children and teenagers are more flexible due to a higher proportion of collagen in their bone matrix.
Physiotherapy:
Physiotherapy for greenstick fractures focuses on gentle range of motion exercises to prevent stiffness and promote healing. It also involves strengthening exercises as the child’s condition improves.
- Pain Management: Initially, physiotherapy focuses on managing pain and discomfort associated with the fracture. Gentle exercises and modalities like ice and heat therapy can help alleviate pain and swelling.
- Maintaining Range of Motion: Immobilization can lead to stiffness in the affected limb. Physiotherapists work to maintain and gradually improve the joint’s range of motion through passive and active exercises.
- Strengthening Muscles: Muscles around the fractured bone can weaken during immobilization. Physiotherapy includes strengthening exercises to restore muscle tone and prevent muscle atrophy.
- Enhancing Functional Mobility: As healing progresses, physiotherapists design exercises to improve functional mobility, ensuring that the child can use the affected limb effectively in everyday activities.
Playground Falls – Forearm Fractures
Fractures of the forearm, specifically the radius or ulna, are common in children who fall while playing. Child forearm fractures refer to broken bones in the forearm of a child. The forearm consists of two bones, the radius and the ulna, which extend from the elbow to the wrist. These fractures can occur in various ways, such as falling on an outstretched hand, direct impact, or twisting of the forearm.

Child forearm fractures are relatively common and can vary in severity from a mild crack to a complete break. Treatment typically involves immobilizing the forearm with a cast or splint to allow the bones to heal properly. In some cases, more severe fractures may require surgical intervention.
Physiotherapy:
Physiotherapy helps in regaining strength and function in the affected arm through exercises that target wrist, elbow, and shoulder mobility and strength. Here’s how:
- Pain Management: After a fracture, children may experience pain and discomfort. Physiotherapists can employ various techniques, such as gentle exercises and manual therapy, to alleviate pain and reduce muscle stiffness.
- Range of Motion: Immobilization, such as casting or splinting, is often required to allow the fracture to heal properly. However, this can lead to stiffness in the affected arm. Physiotherapy helps children gradually regain their range of motion through tailored exercises and stretches.
- Muscle Strengthening: Muscles around the forearm can weaken during the healing process. Physiotherapists create customized exercise programs to strengthen these muscles, aiding in a faster and more complete recovery.
- Functional Independence: For children, regaining the ability to perform daily activities is essential. Physiotherapists work on restoring functional independence by simulating activities like gripping objects, writing, and playing sports.
- Education and Home Exercise: Physiotherapists educate both children and parents about the importance of continuing exercises at home. This empowers families to contribute to the child’s recovery.
- Psychological Support: Coping with a fracture can be emotionally challenging for children. Physiotherapists provide emotional support, helping young patients stay motivated and positive throughout their recovery journey.
Growth Plate Fracture
These fractures occur at the ends of long bones where growth takes place. A growth plate fracture in children, also known as a physical fracture, occurs when there is a break or injury to the growth plate, which is a soft area near the end of a child’s long bones. These growth plates are responsible for bone growth and development. Growth plate fractures are common in children and adolescents because their bones are still growing.

These fractures can vary in severity, and they can affect the child’s future growth if not treated properly. There are different types of growth plate fractures, including:
- Type I: A separation of the growth plate from the bone.
- Type II: A fracture that runs through part of the growth plate and into the bone.
- Type III: A fracture that goes through the growth plate and into the joint surface.
- Type IV: A fracture that involves both the growth plate and the bone.
- Type V: A crush injury to the growth plate.
Physiotherapy:
Proper physiotherapy is essential to ensure that the injured growth plate heals correctly, preventing deformities. It focuses on gentle exercises and monitoring growth. Physiotherapy can play a crucial role in the recovery process for children with growth plate fractures. The specific approach may vary depending on the severity and location of the fracture, but here are some general considerations:
- Immobilization: Initially, the child may need a cast or brace to immobilize the affected area. Physiotherapy will focus on maintaining joint mobility in adjacent areas to prevent stiffness.
- Range of Motion Exercises: Physiotherapists will gradually introduce a gentle range of motion exercises to prevent muscle atrophy and joint stiffness. These exercises should be tailored to the child’s age and the specific fracture.
- Strength Training: As the healing progresses, the child will work on regaining strength in the injured area. This is important to ensure that the child can return to normal activities safely.
- Balance and Coordination: Balance and coordination exercises may be incorporated to help the child regain functional abilities and prevent future injuries.
- Pain Management: Physiotherapists can also use modalities like ice, heat, or ultrasound to manage pain and reduce inflammation in the affected area.
- Education: Both the child and their parents should be educated on proper movement and activity modification to avoid re-injury.
Supracondylar Humerus Fracture in Children
A supracondylar humerus fracture is a type of elbow fracture that occurs in children. It involves a break in the upper part of the humerus bone, just above the elbow joint. This type of fracture is relatively common in pediatric orthopedics.

Supracondylar fractures are often caused by falls onto an outstretched hand or a direct blow to the elbow. They are more frequent in children due to the flexibility of their bones and the tendency to engage in activities that can lead to such injuries.
Physiotherapy:
Physiotherapy aims to regain normal elbow range of motion and strength through various exercises, often starting with passive movements and progressing to active ones.
Physiotherapy plays a crucial role in the rehabilitation of children with supracondylar humerus fractures. Here are some key points regarding physiotherapy for this condition:
- Initial Immobilization: In the acute phase, the fractured arm is typically immobilized in a cast or splint to allow for proper healing. Physiotherapy does not begin until the fracture has sufficiently healed.
- Pain Management: Physiotherapists help manage pain and discomfort through modalities such as ice, gentle massage, and pain-relieving techniques.
- Range of Motion Exercises: Once the fracture has healed, physiotherapy focuses on regaining the child’s range of motion in the elbow and wrist. Gentle and controlled exercises are used to prevent stiffness.
- Strengthening Exercises: Strengthening exercises help rebuild muscle strength, which may have been lost during the period of immobilization. These exercises are introduced gradually and under supervision.
- Functional Training: The physiotherapist will work on restoring functional activities like reaching, grasping, and lifting objects, to ensure that the child can regain independence in daily tasks.
- Balance and Coordination: Balance and coordination exercises are important, especially if there has been a long period of immobility, to help the child regain their sense of balance and coordination.
- Education and Home Exercise Program: Parents are often educated about exercises and activities they can do at home to support their child’s rehabilitation.
- Follow-Up: Regular follow-up appointments with the physiotherapist and the treating physician are essential to monitor progress and make necessary adjustments to the treatment plan.
- Safeguarding Against Re-Injury: Education on proper techniques and activities to avoid re-injury is crucial to prevent future fractures.
Stress Fractures in Children
Stress fractures result from repetitive stress on a bone and are common in athletes.

Stress fractures in children are small cracks or hairline fractures in bones that typically occur due to repetitive stress or overuse of a particular bone. They are common in physically active children and adolescents, especially those involved in sports like running, gymnastics, or dancing. These fractures often develop gradually and may not always cause immediate pain or noticeable symptoms.
Common signs of stress fractures in children may include:
- Localized pain and tenderness at the site of the fracture.
- Pain that worsens with activity and improves with rest.
- Swelling around the affected area.
- Possible limping or altered gait.
- Discomfort that can be reproduced with pressure or tapping on the bone.
Physiotherapy:
For stress fractures, physiotherapy plays a role in assessing and correcting biomechanical factors contributing to the fracture. It also involves a gradual return to activity plans.
Physiotherapy can play a crucial role in the management of stress fractures in children. Here are some key points regarding physiotherapy for stress fractures in children:
- Rest and Protection: Initially, the primary focus is on rest and protection of the affected area to allow the fracture to heal. Your child may need to use crutches or wear a brace to limit weight-bearing on the affected limb.
- Pain Management: Physiotherapists can help manage pain through modalities such as ice, heat, or ultrasound therapy. They may also teach pain-relieving exercises.
- Mobility and Range of Motion: Once healing begins, the physiotherapist will work on maintaining or improving joint mobility and range of motion in the affected area to prevent stiffness.
- Strengthening Exercises: Gradually, your child will be introduced to specific strengthening exercises to rebuild muscle strength around the affected bone. This helps support the healing process and prevents future injuries.
- Gait Training: If the fracture affects a limb, physiotherapists can assist with gait training to ensure your child walks properly and without pain once the bone is healed.
- Education: Physiotherapists provide education on proper body mechanics and techniques to prevent stress fractures in the future. They may discuss factors like footwear, training intensity, and nutrition.
- Monitoring Progress: Regular follow-up appointments with the physiotherapist are essential to monitor progress and make any necessary adjustments to the treatment plan.
Tibial Fractures in Children
Fractures of the tibia, or shinbone, can occur due to falls or sports injuries. A tibial fracture in children refers to a broken bone in the shinbone, known as the tibia, in a pediatric patient.

This type of fracture can vary in severity, from a hairline crack to a complete break, and it often occurs due to trauma or accidents such as falls or sports injuries. Treatment depends on the specific characteristics of the fracture but may include casting, splinting, or surgery in more severe cases to realign and stabilize the bone to promote proper healing.
Physiotherapy:
Physiotherapy for tibial fractures focuses on gait training, strengthening exercises, and balance work to ensure proper healing and prevention of complications.
Physiotherapy plays a crucial role in the rehabilitation of tibial fractures. The primary goals of physiotherapy for this condition are to promote healing, restore normal function, and prevent complications. Here are some key aspects of physiotherapy for tibial fractures in children:
- Pain Management: Physiotherapists can use various techniques, such as ice therapy and gentle manual techniques, to help manage pain and reduce swelling in the affected area.
- Range of Motion (ROM) Exercises: Early in the healing process, gentle range of motion exercises may be introduced to prevent stiffness in the joints surrounding the fracture site.
- Muscle Strengthening: As healing progresses, physiotherapy includes exercises to strengthen the muscles around the tibia, which helps provide support to the healing bone.
- Weight-Bearing Progression: Physiotherapists will guide the child through a gradual return to weight-bearing activities, starting with partial weight-bearing and progressing to full weight-bearing as the fracture heals.
- Gait Training: Teaching the child to walk correctly with the aid of crutches, walkers, or other assistive devices if necessary, to avoid putting excessive stress on the healing tibia.
- Balance and Coordination: Exercises to improve balance and coordination can help prevent falls and further injury during the recovery period.
- Functional Activities: Physiotherapists work with children to help them regain the ability to perform everyday activities, such as climbing stairs or playing sports, once the fracture is healed.
- Education and Home Exercise Programs: Educating both the child and their parents on the importance of following prescribed exercises and precautions at home is essential for a successful recovery.
- Monitoring Progress: Regular follow-up appointments with the physiotherapist are crucial to monitor the healing process and make necessary adjustments to the rehabilitation plan.
What are the preventions for fractures?
Preventing fractures in children involves various measures:
- Supervision: Always supervise young children during play, especially on playgrounds and near stairs to prevent falls.
- Childproofing: Childproof your home by securing sharp objects, covering electrical outlets, and using safety gates to block stairs.
- Safety Gear: Ensure children wear appropriate safety gear like helmets, and knee and elbow pads when biking, skateboarding, or participating in sports.
- Proper Footwear: Ensure children wear well-fitting, supportive shoes to reduce the risk of tripping.
- Balanced Diet: Promote a balanced diet with sufficient calcium and vitamin D for strong bones.
- Regular Exercise: Encourage physical activity to build strong muscles and bones.
- Education: Teach kids about safety, such as looking both ways before crossing the street and not climbing on furniture.
- Safe Playgrounds: Choose playgrounds with age-appropriate equipment and proper surfacing to cushion falls.
- Proper Handling: Show children how to properly carry heavy backpacks and school bags to prevent strain.
- Regular Check-ups: Schedule regular check-ups with a pediatrician to monitor growth and development.
- Water Safety: Supervise children around pools and other bodies of water, and consider swimming lessons.
- Teach Falling Techniques: Teach kids how to fall safely, tucking and rolling if they do fall.
How do physiotherapists treat fractures?
Physiotherapists play a crucial role in the rehabilitation process after a fracture. Their primary goal is to help patients regain strength, mobility, and function in the affected area. Here’s how they typically treat fractures:
Assessment: The physiotherapist begins by assessing the patient’s condition, taking into account the type and location of the fracture, as well as any surgical interventions.
Immobilization: Initially, the fractured area may be immobilized with a cast, brace, or splint. The physiotherapist ensures that these devices are properly fitted and provides guidance on their care.
Pain management: Physiotherapists help manage pain and discomfort through various techniques, such as manual therapy, modalities like heat or cold therapy, and exercises.
Range of motion exercises: As the fracture heals, physiotherapists prescribe a gentle range of motion exercises to prevent stiffness and promote joint mobility in the surrounding areas.
Strengthening exercises: They design personalized exercise programs to strengthen the muscles around the fracture site and improve overall muscle tone. These exercises gradually progress in intensity as healing allows.
Weight-bearing progression: For weight-bearing fractures, physiotherapists guide patients through a gradual return to activities like walking or standing, ensuring they do not put excessive stress on the healing bone.
Gait training: If needed, physiotherapists help patients relearn how to walk properly and adapt their gait to accommodate any changes caused by the fracture.
Functional training: As healing progresses, physiotherapists focus on restoring functional abilities specific to the patient’s daily life, such as reaching, lifting, and climbing stairs.
Education: Physiotherapists educate patients on proper body mechanics, posture, and techniques to avoid re-injury.
Monitoring progress: Throughout the rehabilitation process, physiotherapists continually assess the patient’s progress and adjust the treatment plan accordingly.
What are the 4 R’s of fracture treatment?
Reduction: This involves aligning the broken bone fragments back into their proper position. The reduction can be closed (manipulating the bone without surgery) or open (requiring surgical intervention).
Fixation: After reduction, the fractured bone may need stabilization to keep it in place during the healing process. Fixation methods can include casts, splints, pins, plates, or screws.
Rehabilitation: Rehabilitation is the process of restoring strength, mobility, and function to the injured area through exercises and physical therapy. It helps the patient regain full use of the affected limb or area.
Recovery: This phase involves allowing the fractured bone to heal naturally over time. Recovery times can vary depending on the type and location of the fracture, but it typically involves rest, protection of the injured area, and regular follow-up with a healthcare provider to monitor progress.
What is the classification of fractures in children?
Fractures in children are classified based on various factors, including the location, type, and extent of the fracture. The classification systems commonly used include:
Salter-Harris Classification: This system is specific to growth plate fractures (physeal fractures) and is categorized into five types (I to V) based on the location of the fracture within the growth plate.
Anatomic Location: Fractures can also be classified by their anatomic location, such as forearm fractures, femur fractures, or hand fractures.
Open vs. Closed: Fractures are categorized as either open (compound) or closed, depending on whether the broken bone has pierced the skin (open) or not (closed).
Type of Fracture: Fractures can be classified by their specific characteristics, such as transverse, oblique, spiral, greenstick, or comminuted fractures, based on the pattern of the break.
Stability: Some fractures are classified by stability, with categories like stable, unstable, or displaced fractures. Stable fractures typically have minimal displacement, while unstable ones have significant displacement.
Mechanism of Injury: Fractures can also be classified based on the mechanism of injury, such as falls, sports-related injuries, or trauma.
I am a highly skilled and experienced content writer with a Doctorate in Therapy degree. With a deep understanding of the human body and a passion for health and wellness. I combines my clinical expertise and writing skills to create valuable and engaging content.



Wow, superb weblog layout! How long have you been running a blog for?
you made running a blog glance easy. The total
glance of your website is wonderful, as well as the content material!
You can see similar here najlepszy sklep
Ahaa, its good dialogue on the topic of this paragraph at this place at this website, I
have read all that, so at this time me also commenting here.
I saw similar here: Sklep online
Hi! Do you know if they make any plugins to help with SEO?
I’m trying to get my blog to rank for some targeted keywords but I’m
not seeing very good gains. If you know of any please share.
Kudos! You can read similar blog here: Dobry sklep