What is Duchenne Muscular Dystrophy?
Duchenne Muscular Dystrophy is a rare genetic disorder characterized by the progressive degeneration of muscle tissue. It primarily affects young boys, with symptoms often appearing between the ages of 3 and 5. DMD is caused by a mutation in the DMD gene, which leads to the absence of a vital muscle protein called dystrophin. This deficiency results in muscle weakness and eventual loss of mobility.
expectancy
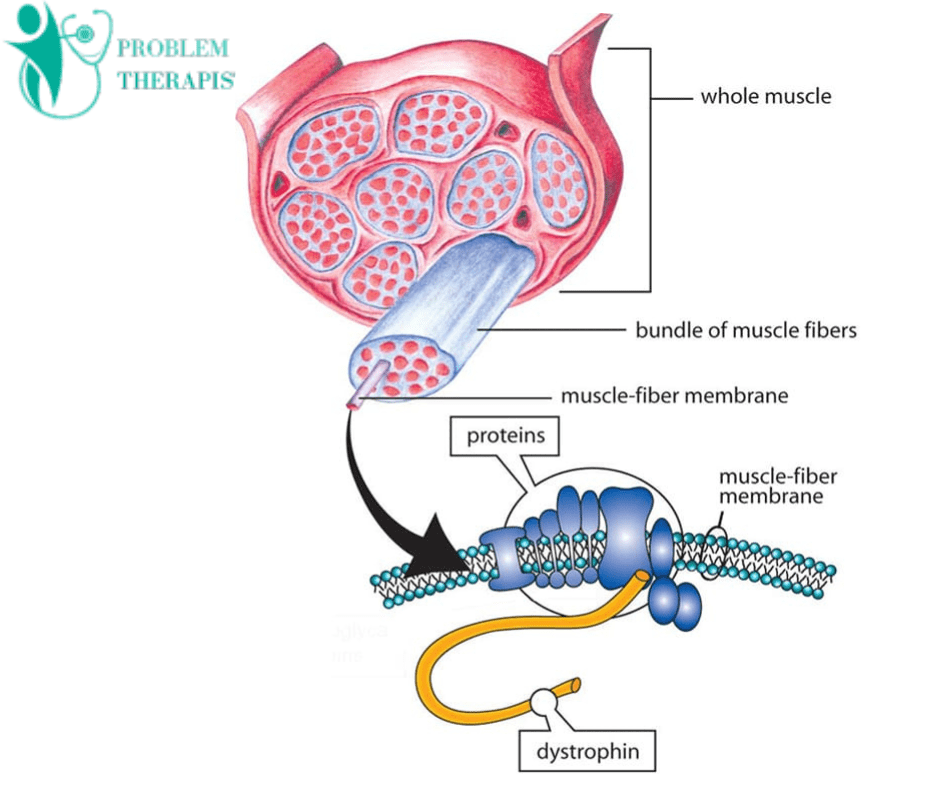
Relevant Anatomy
Duchenne muscular dystrophy (DMD) is a genetic disorder that primarily affects muscle tissue. The related anatomy includes:
- Muscles: DMD primarily impacts skeletal muscles, which are responsible for voluntary movements like walking and lifting objects. Over time, these muscles weaken and deteriorate.
- Dystrophin: The absence or dysfunction of the dystrophin protein is a hallmark of DMD. Dystrophin is crucial for maintaining muscle cell integrity and stability.
- Muscle Fiber: Muscle fibers are the building blocks of muscles. In DMD, muscle fibers undergo damage and degeneration, leading to muscle weakness and atrophy.
- Connective Tissue: Surrounding muscle fibers, there’s connective tissue called fascia. It plays a role in muscle support and protection.
- Nervous System: The nervous system controls muscle movements. DMD doesn’t directly affect the nervous system but impairs muscle function, leading to mobility issues.
- Heart Muscle: DMD can also affect the heart muscle (cardiac muscle), leading to cardiomyopathy and heart problems.
- Bones and Joints: Weak muscles can lead to joint contractures and bone deformities as a result of reduced mobility.
- Respiratory Muscles: DMD can impact the muscles needed for breathing, which can lead to respiratory complications as the disease progresses.
What are the Causes of Duchenne Muscular Dystrophy?
Duchenne muscular dystrophy (DMD) is primarily caused by mutations in the DMD gene. These mutations result in the absence or dysfunction of a protein called dystrophin, which is crucial for muscle cell stability. The main causes include:
- Genetic Mutation: DMD is an inherited genetic disorder caused by mutations in the DMD gene located on the X chromosome.
- X-Linked Recessive Inheritance: DMD primarily affects males because they have only one X chromosome. Females typically carry the mutation as carriers but are often asymptomatic.
- Deletion or Frame-Shift Mutations: Most DMD cases involve large deletions or frame-shift mutations in the DMD gene, leading to non-functional dystrophin protein.
- Lack of Dystrophin: Dystrophin is essential for muscle cell integrity, and its absence or dysfunction causes progressive muscle degeneration.
- Muscle Weakness and Wasting: Without functional dystrophin, muscle fibers weaken, break down, and are replaced by fatty and connective tissue, causing muscle weakness and wasting.
- Progressive Nature: DMD is progressive, leading to loss of mobility and life-threatening complications due to respiratory and cardiac muscle involvement.
- Sporadic Mutations: In some cases, DMD can occur due to spontaneous mutations, not inherited from parents.
What are the Symptoms of Duchenne Muscular Dystrophy?

Here are some common symptoms of Duchenne muscular dystrophy:
- Progressive muscle weakness, typically starting in the legs and pelvis.
- Frequent falls and difficulty getting up from a seated or lying position.
- Delayed motor milestones, such as walking later than usual.
- Waddling gait and difficulty running.
- Muscle stiffness and contractures (tightening of muscles and tendons).
- Difficulty with fine motor skills, like writing or buttoning clothes.
- Enlarged calf muscles (due to muscle fiber replacement with fatty tissue).
- Cardiac issues, as the heart muscle weakens over time.
- Respiratory problems, including difficulty breathing and reduced lung function.
- Cognitive and behavioral challenges, though these are less common and variable.
What are the Early Signs and Diagnosis of Duchenne Muscular Dystrophy?
Early Signs and Diagnosis
Identifying DMD in its early stages is crucial for intervention. Parents and caregivers should be vigilant for signs such as difficulty walking, frequent falls, and delayed motor skills development. A definitive diagnosis is typically made through genetic testing and muscle biopsy.
The diagnosis of Duchenne muscular dystrophy typically involves several steps:
- Clinical Evaluation: A doctor will begin by taking a detailed medical history and performing a physical examination. They will look for signs of muscle weakness, delayed motor milestones, and other characteristic symptoms.
- Blood Tests: Blood tests may be conducted to check for elevated levels of creatine kinase (CK), which is often elevated in individuals with DMD due to muscle damage.
- Genetic Testing: The gold standard for diagnosis is genetic testing, usually through a blood sample. This can identify mutations in the DMD gene responsible for the condition. Techniques such as DNA sequencing and deletion/duplication analysis are commonly used.
- Muscle Biopsy (if needed): In some cases, a small sample of muscle tissue may be taken through a biopsy to confirm the presence of muscle degeneration and to rule out other muscle disorders.
- Electromyography (EMG): EMG measures the electrical activity in muscles and can help differentiate between DMD and other neuromuscular disorders.
- Imaging: Techniques like MRI (Magnetic Resonance Imaging) or ultrasound may be used to visualize muscle tissue and assess its condition.
- Family History: A family history of DMD or related muscular dystrophies can be an important factor in the diagnosis.
What are the Current Treatment Options for Duchenne Muscular Dystrophy?
While there is no cure for DMD, various therapies and treatments aim to manage the condition and improve the quality of life for those affected:
Physical Therapy
Physical therapy plays a central role in the management of Duchenne Muscular Dystrophy. It focuses on maintaining muscle function, preventing contractures, and optimizing mobility. Therapists work with patients to create tailored exercise plans that target specific muscle groups.
Corticosteroids
Corticosteroids, such as prednisone and deflazacort, are commonly prescribed to slow down muscle degeneration and maintain muscle strength. These medications can help delay the progression of the disease.
Assistive Devices
As the condition progresses, individuals with DMD may require assistive devices such as braces, wheelchairs, or mobility aids to enhance their independence and mobility.
Emerging Therapies
The search for more effective treatments for DMD is ongoing. Promising approaches include gene therapy, exon skipping, and stem cell therapy. These cutting-edge treatments offer hope for slowing down the disease’s progression and improving the overall quality of life for those affected.
Coping and Support
Living with Duchenne Muscular Dystrophy can be challenging, both for patients and their families. It is essential to establish a strong support network, access specialized care, and stay informed about the latest advancements in DMD research and treatment options.
DMD Physical Therapy
Physical therapy can help individuals with Duchenne muscular dystrophy (DMD) in several ways:
- Maintaining Muscle Function: Physical therapists design exercise programs to help preserve muscle strength and function, delaying the progression of muscle degeneration.
- Range of Motion: They work on maintaining or improving joint flexibility, and preventing contractures (permanent muscle and joint tightness).
- Respiratory Support: DMD can affect respiratory muscles. Physical therapists teach breathing exercises to improve lung capacity and prevent respiratory complications.
- Mobility: Assistive devices like braces or wheelchairs may be needed. Physical therapists provide training in using these devices safely and effectively.
- Balance and Coordination: DMD can impact balance and coordination. Therapists work on these skills to enhance mobility and prevent falls.
- Pain Management: They employ techniques like massage, stretching, and modalities such as heat or ice to manage pain and discomfort associated with DMD.
- Adaptive Strategies: Physical therapists help patients adapt to daily tasks, making them more manageable and less physically demanding.
- Education: They educate patients and their families on managing symptoms, including the importance of staying active within the individual’s capabilities.
- Functional Independence: The goal is to maximize independence and quality of life, ensuring that individuals with DMD can perform daily activities as long as possible.
- Monitoring Progress: Regular physical therapy sessions allow therapists to assess the progression of DMD and adjust treatment plans accordingly.
Treatment plan
A physical therapy treatment plan for Duchenne muscular dystrophy typically focuses on maintaining and improving mobility, muscle strength, and function while managing symptoms. Here’s a general outline of such a plan:
Initial Assessment
- Comprehensive evaluation of the patient’s current physical condition, muscle strength, joint range of motion, and functional abilities.
- Assessment of any specific muscle weaknesses or contractures.
Individualized Exercise Program For Duchenne Muscular Dystrophy
- Tailored exercise regimen to address specific weaknesses and maintain overall strength.
- Low-resistance exercises, such as swimming, stationary cycling, or gentle resistance training.
- Emphasis on regular stretching to prevent contractures and maintain joint flexibility.
Assistive Devices and Mobility Aids
- Recommendation and training in the use of mobility aids like wheelchairs, braces, or orthotics, as the condition progresses.
- Ensuring proper fit and function of these devices.
Breathing and Respiratory Exercises
- Techniques to improve respiratory muscle strength and function.
- Use of incentive spirometry or other devices to promote deep breathing and lung expansion.
Pain Management
- Strategies to address pain and discomfort may include massage, heat/cold therapy, or positioning.
- Medication management under the guidance of a healthcare provider.
Education and Lifestyle Modifications
- Educating the patient and their family about the condition, its progression, and symptom management.
- Teaching energy conservation techniques to optimize daily activities.
Adaptive Activities
- Recommending adaptive recreational activities that promote social engagement and physical activity.
- Encouraging participation in activities appropriate to the patient’s abilities and interests.
Regular Monitoring
- Periodic re-assessment of the patient’s condition and adjustment of the treatment plan as needed.
- Close collaboration with a multidisciplinary team of healthcare professionals, including physicians, occupational therapists, and nutritionists.
Exercises For Duchenne Muscular Dystrophy
Duchenne muscular dystrophy (DMD) is a progressive genetic disorder that affects muscle strength and function. Exercise should be approached with caution, and it’s essential to consult with a healthcare professional or physical therapist who is familiar with DMD to develop a safe and personalized exercise plan. Exercises may include:
- Range of motion exercises: Gentle movements to maintain joint flexibility and prevent contractures.
- Breathing exercises: To maintain respiratory function and improve lung capacity.
- Hydrotherapy: Water-based exercises in a warm pool can be low-impact and helpful for muscle mobility.
- Stretching: Gentle stretching to prevent muscle tightness and maintain flexibility.
- Assistive devices: Utilizing mobility aids or orthopedic devices to support movement.
- Standing exercises: If possible, supported standing can help with muscle and bone health.
- Low-resistance stationary cycling: This can be beneficial for cardiovascular fitness without excessive strain.
- Occupational therapy: Focusing on activities of daily living and maintaining independence.
- Aquatic therapy: Water-based exercises can provide buoyancy and support for movements.
- Adaptive yoga: Modified yoga poses and breathing exercises to improve flexibility and relaxation.
- Seated exercises: Gentle seated movements to target upper body strength and mobility.
- Electrical stimulation: Under professional guidance, this technique can help maintain muscle function.
What foods should a muscular dystrophy patient avoid?
Individuals with muscular dystrophy may benefit from a balanced and nutritionally sound diet, but it’s important to consult with a healthcare professional or a registered dietitian for personalized guidance. In general, here are some considerations:
- Saturated Fats: Limit saturated fats found in fried foods, fatty cuts of meat, and full-fat dairy as they can contribute to heart health issues, which can be a concern for some individuals with muscular dystrophy.
- Reduce the intake of foods and beverages high in added sugars like sugary drinks, candies, and desserts as they can contribute to weight gain and dental issues.
- Processed Foods: Minimize processed and convenience foods as they often contain high levels of sodium, unhealthy fats, and additives. Fresh, whole foods are generally a better choice.
- Alcohol: It’s advisable to limit or avoid alcohol as it can interact with medications and potentially weaken muscle function further.
- Caffeine: Some individuals may be sensitive to caffeine, which can interfere with sleep and exacerbate fatigue, so moderate consumption may be wise.
- Large Meals: Eating large meals can cause discomfort for those with muscle weakness in the esophagus or digestive tract. Smaller, more frequent meals may be easier to manage.
How can you prevent muscular dystrophy?
Preventive measures for Duchenne muscular dystrophy (DMD) primarily involve genetic counseling and early detection:
- Genetic Counseling: If there is a family history of DMD, consider genetic counseling to assess the risk of passing on the gene mutation to future children.
- Prenatal Testing: For families at risk, prenatal genetic testing can identify the presence of the DMD gene mutation in a developing fetus.
- Carrier Testing: Women with a family history should consider carrier testing to determine if they carry the DMD gene mutation.
- Early Diagnosis: Promptly seek medical evaluation if you suspect DMD in a child. Early diagnosis can lead to better management and interventions.
- Physical Therapy: Physical therapy and exercise can help maintain muscle function and mobility in individuals with Duchenne muscular dystrophy.
- Medications: Consult with a healthcare professional for medications like corticosteroids, which may help slow the progression of DMD symptoms.
- Supportive Care: Provide emotional and psychological support to individuals and families affected by DMD.
Duchenne muscular dystrophy life expectancy 2023
Duchenne muscular dystrophy (DMD) is a genetic disorder characterized by progressive muscle degeneration and weakness. It primarily affects boys and is caused by mutations in the dystrophin gene. DMD is a severe form of muscular dystrophy, and unfortunately, it is associated with a shortened life expectancy.
In the past, individuals with Duchenne muscular dystrophy often did not survive beyond their teenage years or early twenties. However, advancements in medical care, including respiratory support and cardiac management, have improved the life expectancy of individuals with DMD.
What are the recommendations for Duchenne muscular dystrophy?
Someone with Duchenne muscular dystrophy (DMD) can engage in moderate exercise but should avoid reaching the point of exhaustion. Many experts suggest swimming and water exercises (aquatic therapy) as effective ways to keep muscles toned without putting excessive stress on the body.
What is the most effective treatment for muscular dystrophy?
There is currently no cure for muscular dystrophy. Treatment focuses on managing symptoms, physical therapy, and supportive measures to improve quality of life.
Is muscular dystrophy genetic?
Yes, muscular dystrophy is often genetic. It is caused by mutations in genes that are involved in muscle function. There are various types of muscular dystrophy, each associated with specific genetic factors.
What organs are affected by muscular dystrophy?
Muscular dystrophy primarily affects skeletal muscles, which are responsible for voluntary movement. However, the specific muscles affected can vary depending on the type of muscular dystrophy. Commonly affected muscles include those in the legs, arms, and torso. Over time, muscle weakness and wasting can lead to mobility issues and affect the respiratory and cardiac muscles in some cases. It’s important to note that there are several types of muscular dystrophy, each with its own unique characteristics and organ involvement.
What is the most serious form of muscular dystrophy?
The most serious form of muscular dystrophy is Duchenne muscular dystrophy (DMD). It is a genetic disorder characterized by progressive muscle degeneration and weakness, typically affecting boys in childhood. DMD is more severe compared to other forms of muscular dystrophy and often leads to significant disability and a shorter lifespan.
I am a highly skilled and experienced content writer with a Doctorate in Therapy degree. With a deep understanding of the human body and a passion for health and wellness. I combines my clinical expertise and writing skills to create valuable and engaging content.


Wow, awesome weblog structure! How lengthy have you been running a blog for?
you make blogging glance easy. The total look of your website is magnificent, as neatly as
the content! You can see similar here sklep internetowy
Its like you learn my thoughts! You appear to
know so much approximately this, such as you wrote the e book in it or something.
I believe that you could do with some p.c.
to power the message house a bit, however other than that, that is excellent blog.
A great read. I’ll definitely be back. I saw similar here: Sklep internetowy
It’s very interesting! If you need help, look here: ARA Agency
great article
Hey! Do you know if they make any plugins to assist with
Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good gains.
If you know of any please share. Appreciate it! I saw similar art here: Escape rooms review
I have been surfing on-line greater than 3 hours lately, yet I by no means found any interesting article like yours. It’s pretty price enough for me. In my view, if all site owners and bloggers made good content as you did, the net shall be a lot more useful than ever before!
Good post. I learn something totally new and challenging on blogs I stumbleupon on a daily basis. It’s always interesting to read articles from other authors and use a little something from other sites.
I’m very pleased to uncover this page. I want to to thank you for ones time for this particularly fantastic read!! I definitely savored every little bit of it and i also have you saved as a favorite to look at new stuff on your blog.
This constantly amazes me exactly how bloggers such as yourself can find some time and also the dedication to carry on creating good blogposts. Your blog isgood and one of my own must read weblogs. I just wanted to thank you.
This page certainly has all the info I wanted concerning this subject and didn’t know who to ask.
Good post. I learn something totally new and challenging on sites I stumbleupon everyday. It will always be interesting to read through content from other authors and use something from other sites.
Hello there! Do you know if they make any plugins to assist with Search Engine Optimization? I’m trying to get my blog to rank for some targeted keywords but I’m not seeing very good results.
If you know of any please share. Thank you! You can read similar text here
A motivating discussion is worth comment. There’s no doubt that that you ought to write more about this issue, it may not be a taboo subject but typically people do not discuss these topics. To the next! Many thanks.
Very easily, the post is really the greatest on this precious topic. I harmonise with your conclusions and also definitely will thirstily look forward to your incoming updates. Simply just saying thanks can not simply just be enough, for the extraordinary lucidity in your writing. I definitely will quickly grab your rss feed to stay abreast of any kind of updates. Genuine work and much success in your business endeavors!
my English teacher hate me cause i keep writing about somebody from The WANTED called Jay, she gives me evils and low
Greetings I am so thrilled I found your site, I really found you by mistake, while I was searching on Aol for something else, Anyhow I am here now and would just like to say kudos for a remarkable post and a all round thrilling blog (I also love the theme/design), I don’t have time to look over it all at the moment but I have saved it and also added in your RSS feeds, so when I have time I will be back to read a great deal more, Please do keep up the superb job.
Saved as a favorite, I love your website.
I can’t tell you how impressed I am with your article. Your insight and unique ideas have inspired me to think about many things contain here. Thanks for this info.
An outstanding share! I have just forwarded this onto a friend who was doing a little research on this. And he actually bought me dinner simply because I found it for him… lol. So allow me to reword this…. Thank YOU for the meal!! But yeah, thanx for spending some time to talk about this subject here on your web page.
I do accept as true with all the concepts you have offered in your post. They are really convincing and can definitely work. Still, the posts are too brief for novices. Could you please lengthen them a little from next time? Thanks for the post.
I am curious to find out what blog system you’re utilizing? I’m having some minor security issues with my latest site and I’d like to find something more secure. Do you have any recommendations?
Its like you read my mind! You seem to know so much about this, like you wrote the book in it or something. I think that you could do with a few pics to drive the message home a little bit, but instead of that, this is excellent blog. A fantastic read. I’ll definitely be back.
As being a Newbie, We’re permanently exploring online for articles which can be of help to me. Many thanks
Oh my goodness! an amazing post dude. Thank you Nevertheless We are experiencing issue with ur rss . Do not know why Cannot register for it. Is there any person obtaining identical rss dilemma? Anyone who knows kindly respond. Thnkx
This site was… how do I say it? Relevant!! Finally I’ve found something which helped me. Many thanks.
I?ve recently started a blog, the information you offer on this website has helped me greatly. Thank you for all of your time & work.
The next time I read a blog, I hope that it does not disappoint me as much as this particular one. After all, Yes, it was my choice to read through, but I really believed you would have something helpful to say. All I hear is a bunch of moaning about something you could possibly fix if you weren’t too busy searching for attention.
Świetna lektura! Ważne jest, by szerzyć świadomość na temat zagrożeń SEO.
Dzięki za praktyczne wskazówki dotyczące znalezienia wykwalifikowanego specjalisty SEO.
Dzięki za podkreślenie znaczenia profesjonalnego podejścia do SEO.
Doceniam szczegółowe wyjaśnienia i porady dotyczące SEO.
To była otwierająca oczy lektura na temat ryzyk i procesu SEO.
Doceniam skupienie się na zagrożeniach SEO i potrzebie ich usunięcia.
acer laptops have much brighter lcd screens compared to other brands..
you can always count on search engine marketing if you want to promote products online.
Excellent read, I just passed this onto a friend who was doing a little research on that. And he just bought me lunch because I found it for him smile Therefore let me rephrase that: Thank you for lunch!
Have you ever considered about contributing on additional web-sites? may well some great content right here and I’m positive you could share a fantastic deal more if you wrote some content throughout other web sites. You’ll discover a great deal of associated web sites to check out. Only one thing to think about. I’m glad I know about it at least.
This is an amazing blog; I was trying to figure out how to keep in contact with your blog until I find out a decent iphone app for reading wordpress blogs. I really wish you to have a good day and keep with the good work!
There a few fascinating points in time in this post but I don’t know if I see these center to heart. There may be some validity but I’ll take hold opinion until I explore it further. Excellent article , thanks and then we want a lot more! Put into FeedBurner too
I was questioning occasion you ever considered altering layout , design from the website? Its really correctly created; I enjoy what youve obtained to mention. But possibly it is possible to small far more with respect to content so males could interact with it greater. Youve obtained a terrible total lots of text for only getting a single or two images. Maybe you’ll be capable of area out greater?
After study a couple of of the blog posts in your web site now, and I actually like your means of blogging. I bookmarked it to my bookmark web site listing and will be checking again soon. Pls check out my website as nicely and let me know what you think.
This is good-looking appealing , i was searching for somewhat but found your site as a substitute through Google . I be in love with networking. Anyways, really wanted in the direction of drop through and say hello . i have subscribed in the direction of your site plus i am hunting onward in the direction of the updates , Gratitude…
Once I initially commented I clicked the -Notify me when new feedback are added- checkbox and now every time a comment is added I get four emails with the same comment. Is there any means you may remove me from that service? Thanks!
I am glad for writing to let you know of the great experience my friend’s girl went through reading the blog. She figured out several pieces, most notably how it is like to have a great helping style to get many more smoothly completely grasp several specialized issues. You really did more than visitors’ expectations. Thank you for displaying those good, dependable, explanatory and in addition cool guidance on this topic to Lizeth.
Hey there ~ Great stuff, will definitely come back very soon ! My AV
Hmm is anyone else having problems with the pictures on this blog loading? I’m trying to find out if its a problem on my end or if it’s the blog. Any feed-back would be greatly appreciated.
A person necessarily help to make critically posts I’d state. That is the first time I frequented your web page and to this point? I amazed with the analysis you made to create this actual submit incredible. Excellent process!
That’s a good perspective, yet isn’t make any kind of sence in any way talking about of which mather. Just about any technique thank you in addition to pondered try to share a person’s article directly into delicius nonetheless it appears to be problems together with your blogs is it possible to please recheck it. thanks once again.
I am curious to find out what blog platform you happen to be using? I’m experiencing some minor security problems with my latest site and I’d like to find something more safe. Do you have any recommendations?
It really is nice to definitely dig up an internet site the location where the blogger is clever. Thanks for creating your site.
There a few intriguing points over time here but I do not determine if I see they all center to heart. There may be some validity but Let me take hold opinion until I look into it further. Very good write-up , thanks and now we want more! Combined with FeedBurner likewise
when we got our baby, our first priority is to give them the best baby care that we could give.,
Hello, i think that i saw you visited my weblog thus i came to “return the favor”.I’m trying to find things to improve my web site!I suppose its ok to use some of your ideas!!
Your writing is both informative and engaging.공무원 대출
I appreciate your honesty and transparency.구글SEO
I’m very happy to discover this web site. I need to to thank you for ones time due to this fantastic read!! I definitely savored every bit of it and i also have you book marked to see new information in your site.
Spot on with this write-up, I really feel this amazing site needs a lot more attention. I’ll probably be returning to see more, thanks for the advice.
What a lovely blog page. I will certainly be back again. Please keep writing!
A polite letter is important addressed to the magazine’s Fiction Editor, introducing yourself and attaching your story, with double spaced text and having big margins on both sides. This really for ease of use by the magazine staff and is essential. Pages ought to each be numbered.
Employee relations should be given more importance in an office environment as well as on any other business establishment`
This is a topic that’s close to my heart… Best wishes! Where can I find the contact details for questions?
I was able to find good info from your content.
I’m impressed, I have to admit. Seldom do I encounter a blog that’s both educative and engaging, and without a doubt, you’ve hit the nail on the head. The problem is an issue that not enough men and women are speaking intelligently about. Now i’m very happy I found this during my search for something regarding this.
This is a great tip particularly to those new to the blogosphere. Short but very accurate info… Many thanks for sharing this one. A must read article.
This site was… how do I say it? Relevant!! Finally I’ve found something which helped me. Thanks.
I needed to thank you for this very good read!! I absolutely loved every little bit of it. I have you bookmarked to look at new things you post…
An impressive share! I have just forwarded this onto a colleague who has been doing a little homework on this. And he in fact ordered me breakfast simply because I discovered it for him… lol. So let me reword this…. Thank YOU for the meal!! But yeah, thanks for spending the time to discuss this issue here on your site.
Your style is unique in comparison to other folks I have read stuff from. Thanks for posting when you have the opportunity, Guess I will just bookmark this page.
Very nice write-up. I definitely love this site. Keep writing!
I’m sharing this with my friends right away.검색엔진최적화 회사
Howdy! This blog post could not be written much better! Looking through this post reminds me of my previous roommate! He continually kept talking about this. I am going to forward this article to him. Pretty sure he will have a very good read. Thanks for sharing!
This is the perfect site for everyone who hopes to understand this topic. You understand a whole lot its almost hard to argue with you (not that I really would want to…HaHa). You certainly put a fresh spin on a topic which has been discussed for a long time. Wonderful stuff, just great.
Hi, I do believe this is an excellent website. I stumbledupon it 😉 I’m going to come back once again since I book marked it. Money and freedom is the best way to change, may you be rich and continue to guide others.
Nice post. I learn something new and challenging on sites I stumbleupon on a daily basis. It will always be interesting to read content from other writers and use a little something from other sites.
Great article! We will be linking to this great content on our site. Keep up the good writing.
Hi, I do believe this is a great site. I stumbledupon it 😉 I may revisit yet again since i have book marked it. Money and freedom is the best way to change, may you be rich and continue to guide other people.
Having read this I thought it was extremely informative. I appreciate you finding the time and energy to put this short article together. I once again find myself personally spending a significant amount of time both reading and leaving comments. But so what, it was still worth it!
Very good article! We will be linking to this great content on our website. Keep up the good writing.
Very good article. I’m dealing with a few of these issues as well..
Nice post. I learn something totally new and challenging on blogs I stumbleupon every day. It’s always helpful to read through content from other authors and practice a little something from their web sites.
Good information. Lucky me I came across your site by accident (stumbleupon). I’ve saved as a favorite for later!
Throughout World Warfare II, new 4-engine land planes were
developed, and flying boats stopped carrying scheduled passengers out of recent York after 1947.
The final Pan American flight left the terminal in February 1952, sure for Bermuda.
You made some really good points there. I looked on the web for more information about the issue and found most people will go along with your views on this website.
Spot on with this write-up, I actually feel this site needs much more attention. I’ll probably be back again to read through more, thanks for the advice!