Parkinson’s disease (PD) is a neurodegenerative disorder characterized by a range of motor symptoms, with gait disturbances, that is called Parkinson’s gait being a common and impactful manifestation. This article delves into the intricacies of Parkinson’s gait and explores the role of physical therapy in managing and improving this aspect of the condition.
What is Parkinsonian Gait?
Parkinson’s gait:
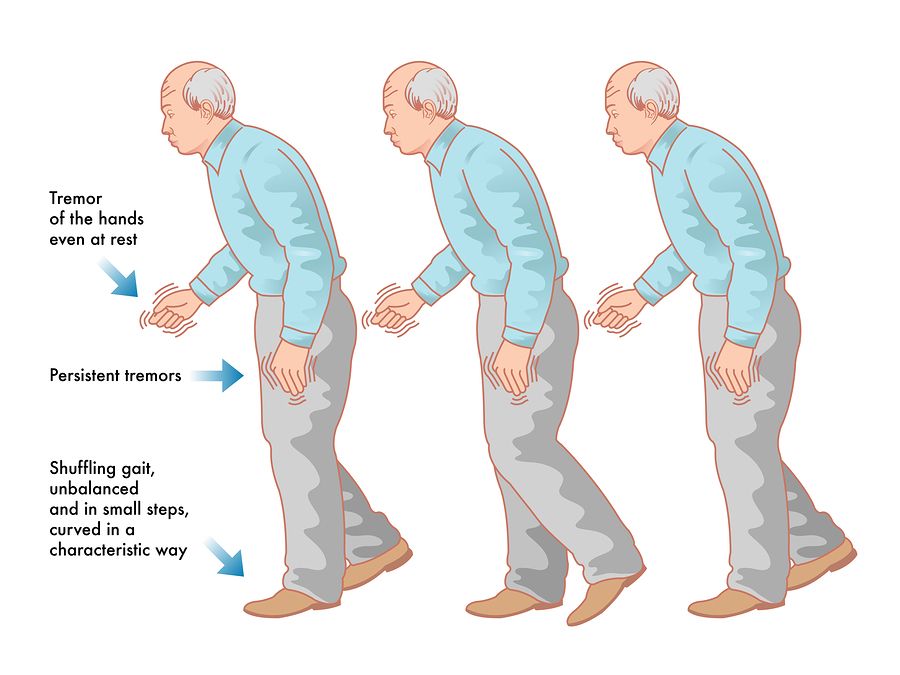
Parkinsonian gait is characterized by a slow, shuffling walking pattern with short steps. People with Parkinson’s may also experience difficulty starting or stopping walking, turning, and maintaining balance. This can lead to an increased risk of falls, which can significantly impact quality of life.
Causes:
Parkinson’s disease is caused by the loss of dopamine-producing cells in the brain. Dopamine is a neurotransmitter that plays an important role in movement control. When dopamine levels are low, it becomes difficult for the brain to send signals to the muscles, leading to the movement problems associated with Parkinson’s disease, including Parkinsonian gait.
Other conditions:
Other conditions that can cause similar gait abnormalities include:
- Lewy body dementia
- Multiple sclerosis
- Stroke
- Brain tumours
- Normal pressure hydrocephalus
Symptoms:
The symptoms of Parkinsonian gait can vary from person to person, but some of the most common symptoms include:
- Small, shuffling steps
- Slow walking speed
- Reduced arm swing
- Stooped posture
- Difficulty initiating walking
- Difficulty turning
- Freezing of gait (sudden inability to move)
- Balance problems
What are the impact and characteristics of Parkinson’s gait?
Impact of Parkinsonian Gait:
- Reduced mobility: People with Parkinson’s gait often take smaller, shuffling steps and walk more slowly. This can make it difficult to keep up with others, navigate busy areas, and complete daily activities.
- Increased risk of falls: The changes in gait and balance associated with Parkinson’s disease make people more likely to fall. Falls can lead to serious injuries, such as broken bones, which can further limit mobility and independence.
- Reduced quality of life: The limitations imposed by Parkinson’s gait can make it difficult to participate in activities that were once enjoyed, such as socializing, traveling, and exercising. This can lead to feelings of isolation, depression, and anxiety.
Parkinson’s Gait Characteristics:
- Shuffling Steps: Individuals with Parkinson’s gait often exhibit a shuffling gait, characterized by short and hesitant steps.
- Reduced Arm Swing: A diminished or absent arm swing is a notable feature, contributing to an overall reduction in balance and coordination.
- Freezing of Gait (FoG): Sudden, brief episodes where a person feels as though their feet are glued to the ground, impeding forward movement.
Mechanisms:
- Dopaminergic Deficiency: Parkinson’s gait abnormalities are primarily attributed to the loss of dopamine-producing cells in the brain, affecting motor control and coordination.
- Postural Instability: Decline in postural reflexes increases the risk of falls, necessitating interventions to enhance stability.
What is the role of physical therapy in Parkinson’s gait treatment?
Physical Therapy Interventions:
Balance Training:
Balance training for Parkinson’s gait is a crucial part of managing the disease and improving quality of life. It focuses on exercises that strengthen muscles, enhance coordination, and boost confidence in maintaining stability while walking and standing.
Benefits:
Here’s how it benefits Parkinson’s gait:
- Improves postural control: Parkinson’s disease often affects posture and balance due to rigidity, tremor, and dopamine deficiency. Balance training strengthens core and leg muscles, allowing for better alignment and control over body movements.
- Enhances gait stability: Gait in Parkinson’s can be characterized by shuffling steps, freezing episodes, and reduced arm swing. Specific exercises target these issues, promoting larger strides, improved arm coordination, and smoother transitions during walking.
- Reduces falls risk: Falls are a significant concern for people with Parkinson’s. Balance training increases confidence and awareness of body position, leading to quicker reflexes and better responses to sudden changes in posture or environment.
- Boosts mental well-being: Exercise itself has mood-lifting effects, and mastering balance exercises can significantly boost self-confidence and independence, enhancing overall well-being for people with Parkinson’s.
Types of balance training:
Static balance exercises:
Here are some static balance exercises that can be beneficial for people with Parkinson’s gait:
- Standing with feet shoulder-width apart: This is a basic but effective exercise. Stand tall with your feet shoulder-width apart and hold for 30 seconds. You can make it more challenging by closing your eyes (if safe to do so) or by focusing on a point on the wall.
- Standing with feet together: This exercise challenges your balance by reducing your base of support. Stand tall with your feet together and hold for 30 seconds.
- Single leg stand: This exercise strengthens your ankles and improves balance on one leg. Stand tall with your feet shoulder-width apart, then slowly lift one foot off the ground and hold for 10 seconds. Repeat on the other side. As you get stronger, you can try holding for longer or closing your eyes (if safe).
- Wall leans: This exercise helps with postural awareness and core strength. Stand with your back against a wall with your feet shoulder-width apart. Slowly lean away from the wall until your heels are a few inches off the ground, then press back into the wall. Repeat 10 times.
Additional Tips:
Here are some additional tips for performing static balance exercises:
- Start slow and gradually increase the difficulty as you get stronger.
- Focus on maintaining good posture with your shoulders back and down and your core engaged.
- Breathe slowly and evenly throughout the exercise.
- Perform the exercises on a soft surface, such as a mat, to reduce the risk of injury in case you lose your balance.
- If you feel dizzy or lightheaded, stop the exercise and rest.
Dynamic balance exercises:
Here are some examples of dynamic balance exercises that can be beneficial for people with Parkinson’s gait:
- Walking with Turns: Start by walking heel-to-toe in a straight line. Gradually progress to incorporating turns, such as walking around cones or squares placed on the floor.
- Turning and Reaching: Stand with feet shoulder-width apart. Practice turning your torso to one side while reaching your arm out in the opposite direction. Slowly return to center and repeat on the other side.
- Backward Walking: Start by walking backward for short distances while holding onto a sturdy surface for support. As balance improves, gradually try walking backward without support.
- Side Stepping: While standing with feet shoulder-width apart, take small steps to the side, leading with one foot at a time. Focus on maintaining good posture and keeping your core engaged.
- Marching in Place: Lift your knees higher than usual while marching in place. This exercise helps with leg coordination and balance.
Important Safety Considerations:
- It’s important to consult with a doctor or physical therapist before starting any new exercise program, especially if you have Parkinson’s disease.
- Perform exercises in a clear, uncluttered space with a sturdy surface nearby for support if needed.
- Start slowly and gradually increase the difficulty of the exercises as your balance improves.
- Listen to your body and take breaks when needed.
- A caregiver or spotter can be helpful, especially when starting new exercises.
Functional balance exercises:
Parkinson’s disease can impact balance, but there are exercises that can help. Here are some functional balance exercises for people with Parkinson’s.
Before You Start:
- Safety first: It’s important to consult a doctor before starting any exercise program, especially if you have Parkinson’s. They can advise on exercises suitable for your condition and recommend a physical therapist who can create a personalized plan.
- Listen to your body: Start slow and gradually increase the difficulty as you get stronger. Take breaks when needed and stop if you experience any pain.
- Focus on good form: It’s more important to do the exercises correctly than quickly.
Exercises:
Here are some examples of functional balance exercises:
- Standing balance: Stand tall with your feet shoulder-width apart and hold onto a chair or counter for support. Practice shifting your weight from one foot to the other, holding for a few seconds at a time.
- Tandem stance: Stand with one foot directly in front of the other, heel-to-toe. Hold for a few seconds, then switch feet.
- Single leg stand: Stand with your arms by your sides and slowly lift one leg behind you. Hold for a few seconds, then switch legs.
- Side stepping: Take small steps to the side, leading with one foot at a time. Focus on keeping your hips and shoulders facing forward.
- Reaching: Stand with your feet shoulder-width apart and reach out with one arm overhead. Hold for a few seconds, then switch arms. You can also try reaching down towards the floor while keeping your back straight.
- Walking with obstacles: Practice walking around cones or other obstacles placed on the floor. This will help you improve your agility and coordination.
Dual Tasking:
In addition to these exercises, incorporating “dual tasking” into your daily routine can be very helpful. Dual tasking involves performing a cognitive task (like counting backwards) while doing a physical activity (like walking). This mimics the challenges of everyday life and helps improve your ability to multitask safely.
Gait Training:
Therapists work on correcting gait abnormalities, emphasizing longer steps, increased arm swing, and a more natural walking pattern.
There are a number of different gait training exercises that can be beneficial for people with Parkinson’s disease. Some common exercises include:
- Walking with a cue: This can be done with a metronome, music, or visual cues. Cues can help to improve walking speed, stride length, and symmetry.
- Dual tasking: This involves walking while doing another activity, such as talking or carrying an object. Dual tasking can help to improve cognitive function and walking ability.
- Obstacle course training: This can help to improve balance and agility.
Benefits:
Gait training can help to improve these symptoms by:
- Increasing your awareness of your posture and gait
- Strengthening your muscles
- Improving your balance and coordination
- Teaching you new walking strategies
Cueing Techniques:
Cueing training is a type of therapy that uses external cues to help people with Parkinson’s disease improve their gait. Gait refers to the way a person walks, and people with Parkinson’s disease often experience gait problems such as slowness, shuffling, freezing, and difficulty turning.
Cues can be auditory, visual, or tactile, and they provide the person with Parkinson’s gait with information about how to move their body. For example, an auditory cue might be a metronome that clicks at a steady pace, or a visual cue might be a line on the floor that the person can walk on.
There is a growing body of evidence that cueing training can be effective in improving gait in people with Parkinson’s disease. One study found that cueing training improved gait speed, stride length, and cadence in people with Parkinson’s disease. Another study found that cueing training reduced freezing of gait, which is a common and debilitating symptom of Parkinson’s disease.
Types:
Here are some of the different types of cueing training that are used for Parkinson’s gait:
- Auditory cueing: This type of cueing uses sounds, such as music, metronomes, or verbal cues, to help the person with Parkinson’s disease walk at a normal pace and stride length.
- Visual cueing: This type of cueing uses visual cues, such as lines on the floor or marks on the wall, to help the person with Parkinson’s disease walk in a straight line and avoid obstacles.
- Tactile cueing: This type of cueing uses touch, such as taps on the arm or leg, to help the person with Parkinson’s disease initiate movement and take larger steps.
Strength and Flexibility Exercises:
Targeting specific muscle groups enhances strength, flexibility, and overall mobility, contributing to better gait performance.
Here are some strength and flexibility exercises that can help improve gait in people with Parkinson’s gait:
Strength exercises:
- Squats: Squats work multiple muscle groups in the legs, hips, and core, which are all important for good gait. Stand with your feet shoulder-width apart and toes slightly pointed outward. Slowly lower yourself down as if you were going to sit in a chair, keeping your back straight and core engaged. Push yourself back up to starting position. Aim for 10-15 repetitions, 2-3 sets.
- Lunges: Lunges work the muscles in the front and back of your legs. Stand with your feet hip-width apart. Step forward with one leg, lowering your hips until both knees are bent at 90-degree angles. Push yourself back up to starting position and repeat with the other leg. Aim for 10-12 repetitions per leg, 2-3 sets.
- Heel raises: Heel raises strengthen the calf muscles, which are important for pushing off during gait. Stand tall with your feet shoulder-width apart. Slowly raise your heels off the ground as high as you can, then slowly lower them back down. Aim for 15-20 repetitions, 2-3 sets.
- Side leg lifts: Side leg lifts strengthen the hip abductors, which help to stabilize the pelvis during gait. Lie on your side with your legs stacked on top of each other. Slowly lift your top leg up as high as you can without pain, then lower it back down. Aim for 10-12 repetitions per leg, 2-3 sets.
Flexibility exercises:
- Hamstring stretch: Sit on the floor with your legs extended straight out in front of you. Lean forward from your hips, reaching your hands toward your toes. If you can’t reach your toes, don’t worry, just reach as far as you can comfortably. Hold for 30 seconds.
- Calf stretch: Stand facing a wall and place your hands shoulder-width apart on the wall at eye level. Step one leg back and keep your heel flat on the floor. Lean forward until you feel a stretch in your calf. Hold for 30 seconds, then switch legs.
- Quadriceps stretch: Stand holding onto a chair or wall for balance. Bend one leg back and grab your foot with your hand, pulling your heel up towards your buttocks. Hold for 30 seconds, then switch legs.
- Hip flexor stretch: Kneel on one knee with the other foot flat on the floor in front of you. Lean forward from your hips, keeping your back straight, until you feel a stretch in your hip flexor. Hold for 30 seconds, then switch sides
Dual-Task Training:
Integrating cognitive tasks during physical activities helps individuals manage gait and multitask more effectively.
- Training involves practicing walking while engaging in various secondary tasks. These tasks can range from simple verbal counting or reciting aloud to more complex activities like carrying objects, navigating obstacles, or performing mental calculations.
- The difficulty of the secondary tasks is gradually increased as the person progresses through the training program. This helps them develop the cognitive and motor skills needed to prioritize and coordinate multiple tasks simultaneously.
Examples:
- Walking on a treadmill while performing verbal fluency tasks.
- Walking over obstacles while carrying objects.
- Walking and talking simultaneously.
- Attending to auditory cues while walking.
Conclusion:
Parkinson’s gait significantly impacts the quality of life for individuals with the disease. A multidisciplinary approach, with physical therapy at its core, proves instrumental in addressing and managing these challenges. As research continues to unfold, a deeper understanding of Parkinson’s gait mechanisms will pave the way for more targeted and effective therapeutic interventions.
FAQ’s:
How do you manage gait in Parkinson’s?
Managing gait in Parkinson’s disease involves a multi-pronged approach that includes medication, physical therapy, and lifestyle changes.
Medication:
The primary medications used to treat Parkinson’s disease, such as levodopa, can help improve gait by increasing dopamine levels in the brain. However, the effectiveness of medication can wear off over time, leading to fluctuations in gait.
Physical Therapy:
Physical therapy plays a crucial role in gait management for Parkinson’s disease. A physical therapist can design a personalized exercise program that includes:
- Flexibility exercises to improve range of motion in the joints.
- Strength training to improve muscle strength and coordination.
- Balance training to improve stability and prevent falls.
- Gait training to practice walking with good posture, stride length, and arm swing.
Lifestyle Changes
Several lifestyle changes can also help manage gait in Parkinson’s disease:
- Regular exercise: Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Good posture: Practice standing tall with your shoulders back and your head held high.
- Assistive devices: Using a cane or walker can help improve balance and safety.
- Proper footwear: Wear well-fitting shoes with good support.
- Physical therapy at home: Practice the exercises your physical therapist teaches you at home regularly.
Additional Strategies:
- Cueing: Using visual, auditory, or somatosensory cues can help improve gait in people with Parkinson’s disease. Visual cues include lines on the floor or following a laser line. Auditory cues include using a metronome or music to pace walking. Somatosensory cues include using textured insoles or vibrating insoles in shoes.
- Action observation and motor imagery: This involves visualizing yourself walking normally or watching someone else walk and imitating their gait.
How do you treat shuffling gait in Parkinson’s?
Shuffling gait, a common symptom of Parkinson’s disease, is characterized by small steps, where the feet drag along the ground rather than lifting completely. Here are some ways to treat shuffling gait in Parkinson’s:
- Medication: Levodopa, the main medication for Parkinson’s gait, can help improve gait in some people. It works by increasing dopamine levels in the brain.
- Physical therapy: A physical therapist can teach exercises to improve strength, flexibility, balance, and coordination. These exercises can help people with Parkinson’s walk more safely and efficiently.
- Assistive devices: Canes, walkers, and other assistive devices can help people with Parkinson’s maintain balance and stability.
Additional Tips:
Here are some additional tips that may help improve shuffling gait:
- Focus on taking larger steps. This can help to improve stride length and overall walking speed.
- Swing your arms as you walk. This can help to improve coordination and balance.
- Walk to a beat. Listening to music or using a metronome can help to cue your steps and improve gait rhythm.
- Practice walking heel-toe. This can help to improve foot clearance and prevent shuffling.
What vitamin stopped shaking in Parkinson’s?
There is no single vitamin that has been proven to stop shaking in Parkinson’s disease. Parkinson’s disease is a complex neurological disorder that affects the part of the brain that controls movement. There is no cure for Parkinson’s disease, but there are medications that can help to manage the symptoms.
However, some studies suggest that certain vitamins, such as vitamin D, B complex vitamins, and Coenzyme Q10, may help to reduce the severity of tremors and other symptoms of Parkinson’s disease. These studies are ongoing, and more research is needed to confirm these findings.
If you are considering taking vitamins or supplements to help manage your Parkinson’s disease, it is important to talk to your doctor first. They can help you determine if vitamins or supplements are right for you and can recommend the appropriate dosage.
I am a highly skilled and experienced content writer with a Doctorate in Therapy degree. With a deep understanding of the human body and a passion for health and wellness. I combines my clinical expertise and writing skills to create valuable and engaging content.