Endometriosis is a complex and often painful condition that affects millions of women worldwide. Despite its prevalence, it remains widely misunderstood. In this article, we’ll delve into the causes, symptoms, and treatment options for endometriosis, shedding light on this often overlooked disorder.
What is endometriosis?
Endometriosis:
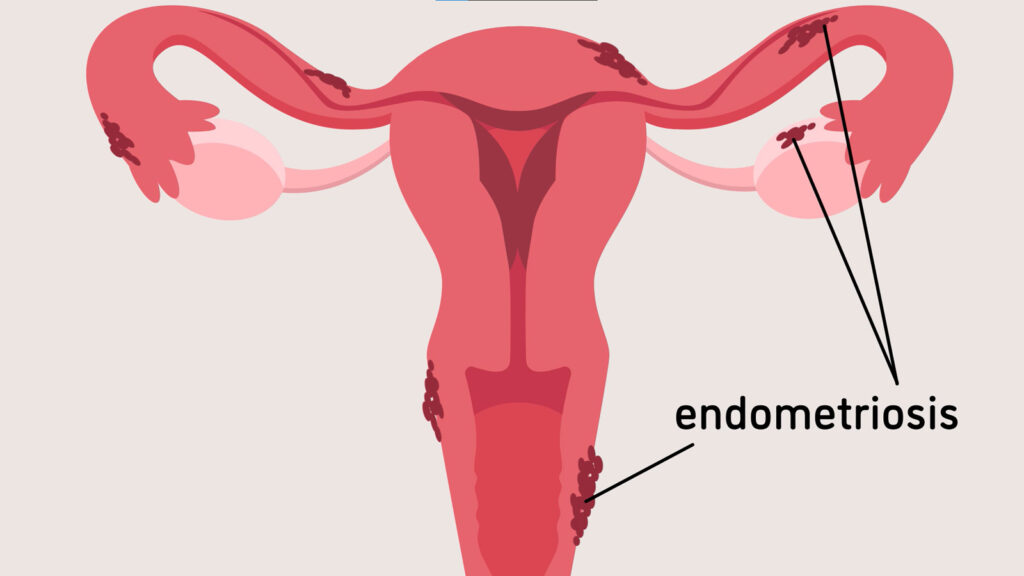
Endometriosis is a condition that affects millions of women worldwide. It occurs when tissue similar to the lining of the uterus (endometrium) grows outside the uterus, most commonly in the pelvic region. This misplaced tissue responds to hormonal changes during the menstrual cycle, just like the endometrial lining inside the uterus. However, unlike the lining that sheds during menstruation, the endometrial tissue outside the uterus has no way to leave the body. This can lead to inflammation, pain, and scar tissue formation.
What are different stages of endometriosis?
Stages:
Endometriosis is a condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus. This tissue can be found on the ovaries, fallopian tubes, and other tissues lining the pelvis. Endometriosis stages are classified based on the extent of the endometrial implants, where they are located, and the presence of scar tissue (adhesions).
The American Society for Reproductive Medicine (ASRM) classifies endometriosis into four stages:
- Stage I (Minimal):This is the mildest stage of endometriosis. There are few small implants, usually superficial (on the surface) of the pelvic organs or lining of the pelvis. There is little to no scar tissue.
- Stage II (Mild): There are more implants and some may be deeper than in stage I. There may be early signs of scarring.
- Stage III (Moderate):There are many implants, some of which may be deep. Scar tissue (adhesions) may be moderate and may partially obstruct pelvic organs. One or both ovaries may have endometriomas (chocolate cysts).
- Stage IV (Severe): There are numerous deep implants throughout the pelvic cavity. Endometriomas and extensive adhesions are also present. This is the most severe stage of endometriosis.
What are causes of endometriosis?
Causes of Endometriosis:
Endometriosis occurs when tissue similar to the lining of the uterus (endometrium) grows outside the uterus. While the exact cause is not fully understood, several factors may contribute to its development:
- Retrograde Menstruation: This occurs when menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of exiting the body. The displaced endometrial cells can then attach to pelvic organs and grow.
- Hormonal Imbalance: Estrogen, a hormone that promotes the growth of the endometrium, may play a role in the development of endometriosis. Imbalances in estrogen levels could contribute to abnormal tissue growth.
- Immune System Disorders: Dysfunction in the immune system may impair the body’s ability to recognize and eliminate endometrial tissue growing outside the uterus.
- Genetic Factors: Endometriosis tends to run in families, suggesting a genetic component to the condition.
What are risk factor of endometriosis?
Here are some risk factors for endometriosis:
Family history:
Having a close relative, such as a mother, sister, or daughter, with endometriosis increases your risk.
Menstrual periods:
- Starting your period at an early age (before age 11)
- Having short menstrual cycles (less than 27 days)
- Having heavy or prolonged menstrual periods (lasting more than seven days)
- Never giving birth
Endometriosis implants after surgery:
In some cases, endometrial tissue can implant itself outside the uterus after pelvic surgery, such as a C-section or myomectomy (removal of uterine fibroids).
Other medical conditions:
Certain medical conditions, such as uterine abnormalities or müllerian anomalies, may increase your risk of endometriosis.
Low body mass index (BMI):
Women with a lower BMI may be at higher risk of endometriosis.
What are symptoms of endometriosis?
Symptoms:
Endometriosis presents a wide range of symptoms, which can vary in severity from one individual to another. Common signs and symptoms include:
- Pelvic Pain: Chronic pelvic pain, often worsening during menstruation, is a hallmark symptom of endometriosis. This pain may also occur during intercourse or bowel movements.
- Menstrual Irregularities: Women with endometriosis may experience heavy or irregular menstrual periods.
- Painful Intercourse: Pain during or after sexual intercourse, known as dyspareunia, is another common symptom of endometriosis.
- Gastrointestinal Symptoms: Some women may experience symptoms such as diarrhea, constipation, bloating, or nausea, especially during menstruation.
- Infertility: Endometriosis can affect fertility, making it difficult for women to conceive.
What ate the complications of endometriosis?
Here are some of the complications of endometriosis:
- Pain: Pelvic pain is the most common symptom of endometriosis. It can occur during your menstrual period, ovulation, or throughout your menstrual cycle. The pain can be sharp, cramping, or a dull ache. You may also experience pain during sexual intercourse, bowel movements, or urination.
- Infertility: Endometriosis can cause infertility in up to half of women with the condition. The inflammation and scar tissue caused by endometriosis can block the fallopian tubes, preventing the egg and sperm from meeting. Endometriosis may also damage the eggs or sperm.
- Adhesions: Endometriosis can cause bands of scar tissue to form around the pelvic organs. These adhesions can cause the organs to stick together, which can lead to pain, bowel obstruction, and other problems.
- Ovarian cysts: Endometriosis can also cause cysts to form on the ovaries. These cysts, called endometriomas, can be painful and may rupture.
Less common, but more serious complications of endometriosis include:
- Damage to an organ: During surgery to treat endometriosis, there is a small risk of damaging an organ, such as the uterus, bladder, or bowel.
- Severe bleeding: In rare cases, endometriosis can cause severe bleeding inside the abdomen.
- Blood clots: Endometriosis can increase your risk of developing blood clots in the legs (deep vein thrombosis) or lungs (pulmonary embolism).
How to treat symptoms of endometriosis?
Treatment Options for Endometriosis:
Treatment for endometriosis aims to relieve symptoms and improve quality of life. The choice of treatment depends on factors such as the severity of symptoms, the desire for fertility, and the individual’s preferences. Treatment options include:
Pain Medication:
It is a condition that can cause significant pain, and managing this pain often requires a multifaceted approach. Here are some common medications and treatments used to alleviate endometriosis-related pain:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Over-the-counter NSAIDs like ibuprofen (Advil, Motrin) and naproxen (Aleve) can help reduce inflammation and alleviate pain.
Hormonal Therapies:
- Birth Control Pills: Oral contraceptives can help regulate or eliminate periods, reducing the frequency and severity of pain.
- Progestins: Medications like medroxyprogesterone (Depo-Provera) and norethindrone can suppress menstruation and growth of endometrial tissue.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: Drugs such as leuprolide (Lupron) and nafarelin (Synarel) reduce estrogen production, creating a temporary menopausal state which can shrink endometrial tissue and reduce pain.
- Aromatase Inhibitors: Medications like letrozole (Femara) and anastrozole (Arimidex) reduce estrogen levels and are sometimes used in combination with other hormonal treatments.
Pain Relievers: For more severe pain, stronger prescription pain medications such as opioids might be necessary. However, these are usually considered a last resort due to the potential for dependency and side effects.
Neuromodulators: Medications typically used for neuropathic pain, such as gabapentin (Neurontin) and pregabalin (Lyrica), can sometimes help with chronic pelvic pain.
Healthy diet:
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside the uterus. This tissue can cause pain, inflammation, and other symptoms. While there is no one-size-fits-all diet for it, there is some evidence that suggests that a healthy, anti-inflammatory diet may help to improve symptoms.
Here are some tips for creating a healthy diet for condition:
- Focus on whole, unprocessed foods. This includes fruits, vegetables, whole grains, lean protein, and healthy fats.
- Eat plenty of fruits and vegetables. Fruits and vegetables are packed with antioxidants and other nutrients that can help to reduce inflammation. Aim for at least five servings per day.
- Choose lean protein sources. Lean protein can help you feel full and satisfied. Good sources of lean protein include fish, poultry, beans, and tofu.
- Include healthy fats in your diet. Healthy fats, such as omega-3 fatty acids, can help to reduce inflammation. Good sources of omega-3 fatty acids include fatty fish, nuts, and seeds.
- Limit processed foods, red meat, and sugary drinks. Processed foods, red meat, and sugary drinks can all contribute to inflammation.
Specific foods:
Here are some specific foods that may be beneficial for people:
- Fatty fish: Salmon, sardines, mackerel, and herring are all good sources of omega-3 fatty acids.
- Fruits and vegetables: Fruits and vegetables are high in antioxidants and fiber, which can help to reduce inflammation.
- Whole grains: Whole grains are a good source of complex carbohydrates, which can help you feel full and satisfied.
- Leafy green vegetables: Leafy green vegetables are a good source of vitamins, minerals, and antioxidants.
- Nuts and seeds: Nuts and seeds are a good source of healthy fats, protein, and fiber.
- Legumes: Beans, lentils, and chickpeas are a good source of plant-based protein and fiber.
Regular exercise:
Regular exercise is a great way to manage endometriosis symptoms, even though there is no cure.
Benefits:
Here are some benefits of exercise:
- Reduces pain: Exercise can help reduce pain by releasing endorphins, which have natural painkilling properties. It can also improve circulation, which can help reduce inflammation.
- Improves mood: Exercise can also help improve mood and reduce stress, both of which can worsen the symptoms.
- Boosts energy levels: Regular exercise can help you feel more energetic, which can be helpful when you’re dealing with fatigue.
Exercises:
Here are some types of exercise that may be beneficial:
- Aerobic exercise: Walking, swimming, and biking are all great options for aerobic exercise. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Yoga: Yoga can help improve flexibility, strength, and balance. It can also help reduce stress and pain. There are many different types of yoga, so you can find one that fits your fitness level and interests.
- Pelvic floor exercises: Pelvic floor exercises can help strengthen the muscles in your pelvic floor, which can help improve bladder control and reduce pain during sex.
Additional Tips:
Here are some tips for getting started with exercise if you have endometriosis:
- Start slowly and gradually increase the intensity and duration of your workouts.
- Listen to your body and take rest days when you need them.
- Choose activities that you enjoy. You’re more likely to stick with an exercise program if you find activities that you find fun.
- Talk to your doctor before starting any new exercise program, especially if you have any concerns.
Stress management:
It is a chronic condition that can cause pain, fatigue, and other symptoms. Stress can also worsen these symptoms. There are a number of things you can do to manage stress and improve your quality of life.
Here are some tips for stress management:
- Mindfulness techniques: Mindfulness techniques, such as deep breathing, meditation, and yoga, can help to reduce stress and promote relaxation. These techniques can help you to focus on the present moment and let go of worries about the past or future.
- Exercise: Regular physical exercise can help to reduce stress, improve mood, and boost overall physical health. Aim for at least 30 minutes of moderate-intensity exercise most days of the week.
- Healthy diet: Eating a healthy, balanced diet can help to reduce stress and improve overall health. Focus on eating plenty of fruits, vegetables, and whole grains. Limit processed foods, sugary drinks, and unhealthy fats.
- Sleep: Getting enough sleep is important for overall health and well-being. Aim for 7-8 hours of sleep each night.
- Support groups: Joining a support group can be a great way to connect with other people who understand what you’re going through. Support groups can provide emotional support, information, and tips for managing it.
- Therapy: A therapist can help you to develop coping mechanisms for dealing with stress and pain.
Alternative therapies:
It is a condition where tissue similar to the lining of the uterus grows outside the uterus. It can cause pain, especially during menstruation, and other problems, such as infertility. While there is no cure for endometriosis, there are a number of alternative therapies that may help to relieve symptoms.
Examples:
Here are some of the most common alternative therapies:
- Acupuncture: Acupuncture is a traditional Chinese medicine technique that involves inserting thin needles into certain points on the body. Studies have shown that acupuncture may be effective in reducing pain associated with endometriosis.
- Herbal medicine: Some herbal remedies, such as those containing turmeric or fish oil, may help to reduce inflammation and pain associated with endometriosis. However, it is important to talk to a healthcare provider before taking any herbal supplements, as they can interact with other medications.
- Diet and exercise: Eating a healthy diet and exercising regularly can help to improve overall health and well-being, which may also help to reduce symptoms. In particular, a diet that is low in inflammatory foods and high in fruits, vegetables, and whole grains may be beneficial.
Hormonal Therapy:
Hormonal therapy is a common first-line treatment for endometriosis. It works by regulating the hormones that cause the endometrial tissue to grow. It is a condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus, most commonly on the ovaries, fallopian tubes, and tissues lining the pelvis.
Benefits:
Here’s how hormonal therapy helps with it:
- Reduces estrogen levels: Estrogen promotes the growth of endometriosis implants. By lowering estrogen levels, hormonal therapy can help shrink these implants and reduce pain.
- Stops menstruation: Endometriosis implants bleed along with the uterine lining during menstruation. Stopping menstruation can significantly improve pain and other symptoms.
Types:
There are different types of hormonal therapies used for it, including:
- Combined oral contraceptive pills: These pills contain both estrogen and progestin. Progestin counteracts the effects of estrogen on endometriosis implants. Birth control pills can be taken continuously to prevent menstruation and reduce symptoms.
- Progestin-only therapy: Progestin can be delivered through various methods, such as pills, injections, intrauterine devices (IUDs), and implants. Progestin thins the uterine lining and reduces menstrual bleeding.
- Gonadotropin-releasing hormone (GnRH) agonists: These medications suppress the production of estrogen by the ovaries, essentially creating a temporary menopause. GnRH agonists are typically used for a short duration due to side effects like bone loss.
Surgery:
Surgery is a potential treatment option for endometriosis, a condition where tissue similar to the lining of the uterus grows outside the uterus. There are two main types of surgery for endometriosis:
- Laparoscopy: This is a minimally invasive surgery that is the most common treatment for endometriosis. During laparoscopy, the surgeon makes small incisions in the abdomen and inserts a thin tube with a light and camera (laparoscope) to see inside the pelvic area. The surgeon can then use small instruments inserted through other incisions to remove or destroy endometriosis implants and scar tissue.
- Laparotomy: This is a major surgery that involves making a larger incision in the abdomen. A laparotomy may be necessary if condition is severe or if laparoscopy is not possible.
The type of surgery you have will depend on the severity of your endometriosis, your symptoms, and your desire for future pregnancy.
Benefits:
Here are some of the benefits of surgery:
- Can improve pain and other symptoms
- May improve fertility
Here are some of the risks of surgery:
- Infection
- Bleeding
- Damage to nearby organs
- Recurrence of endometriosis
Fertility Treatment:
it can cause infertility in some women. The endometrial tissue that grows outside the uterus can interfere with ovulation, fertilization, and implantation. There are a number of fertility treatments that can help women with endometriosis conceive.
- Surgery: Laparoscopic surgery can be used to remove endometriosis implants. This can improve fertility by reducing inflammation and scarring in the pelvis.
- Ovulation induction medications: These medications stimulate the ovaries to produce more eggs. Clomiphene citrate (Clomid) is the most common medication used for ovulation induction.
- Intrauterine insemination (IUI): IUI involves placing sperm directly into the uterus during ovulation. This can increase the chances of sperm fertilizing an egg.
- In vitro fertilization (IVF): IVF is a more complex fertility treatment that involves fertilizing eggs with sperm outside the body. The resulting embryos are then implanted in the uterus. IVF is a good option for women with severe endometriosis or who have not had success with other fertility treatments.
Conclusion:
Endometriosis is a challenging condition that can significantly impact a woman’s physical and emotional well-being. By understanding its causes, symptoms, and treatment options, individuals can work with healthcare providers to develop personalized management plans tailored to their needs. Increased awareness, research, and support are essential in improving the diagnosis and management, ultimately enhancing the quality of life for affected individuals.
FAQ’s:
What happens when a woman has endometriosis?
Endometriosis is a condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus, most commonly on the ovaries, fallopian tubes, and tissues lining the pelvis. This misplaced tissue behaves like the normal endometrial tissue – it thickens, breaks down, and bleeds with each menstrual cycle. However, unlike the endometrial tissue lining the uterus which exits the body during menstruation, this misplaced tissue has no way to escape. This can cause inflammation, pain, and scar tissue formation.
While it is a common gynecological condition, affecting an estimated 1 in 10 women of reproductive age, the symptoms can vary greatly. Some women may experience no noticeable symptoms at all, while others may have severe pain and other problems.
Symptoms:
Here are some of the common symptoms:
- Painful periods (dysmenorrhea)This is the most common symptom of endometriosis. The pain may be severe and can start a few days before your period and last for several days afterwards. It may also radiate to your lower back and thighs.
- Pain during or after sex Sex can be painful for women with endometriosis, especially during deep penetration.
- Painful bowel movements or urination You may experience pain during bowel movements or urination, especially during your period.
- Excessive bleeding You may have heavy periods or bleeding between periods.
- Infertility Endometriosis can sometimes make it difficult to get pregnant.
What is Stage 4 endometriosis?
Stage 4 is the most severe form of the disease. It is characterized by:
- Many deep endometrial implants throughout the pelvic region and abdomen
- Large ovarian endometriomas (chocolate cysts)
- Thick, dense adhesions that can distort pelvic anatomy
The extensive endometrial implants and adhesions can cause a variety of symptoms, including:
- Pelvic pain
- Painful periods
- Pain during intercourse
- Painful bowel movements and urination
- Fatigue
- Infertility
It’s important to note that not everyone with stage 4 endometriosis will have all of these symptoms. Some women may have very few symptoms, while others may have debilitating pain.
Is endometriosis painful?
Yes, it can be very painful. The most common symptom are pelvic pain, which can occur during or outside of your menstrual period.
The pain from endometriosis can vary from woman to woman, but it is often described as a cramping, burning, or aching sensation in the lower abdomen and pelvis. It can also radiate to the lower back and thighs.
For some women, the pain is worse during their periods. For others, the pain is more constant and can occur throughout the month. In some cases, the pain can be so severe that it interferes with daily activities.
I am a highly skilled and experienced content writer with a Doctorate in Therapy degree. With a deep understanding of the human body and a passion for health and wellness. I combines my clinical expertise and writing skills to create valuable and engaging content.


Thank you for the auspicious writeup It in fact was a amusement account it Look advanced to far added agreeable from you However how can we communicate
Very interesting info!Perfect just what I was searching for!Leadership